Search
- Page Path
- HOME > Search
- Diabetes, Obesity and Metabolism
- Incretin and Pancreatic β-Cell Function in Patients with Type 2 Diabetes
- Chang Ho Ahn, Tae Jung Oh, Se Hee Min, Young Min Cho
- Endocrinol Metab. 2023;38(1):1-9. Published online February 13, 2023
- DOI: https://doi.org/10.3803/EnM.2023.103
- 3,333 View
- 362 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
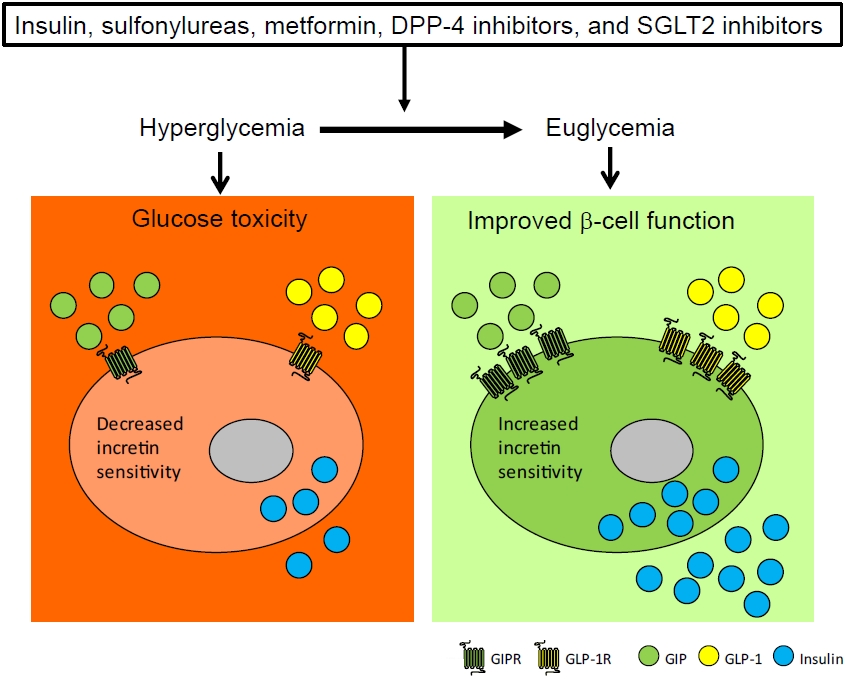
ePub - To maintain normal glucose homeostasis after a meal, it is essential to secrete an adequate amount of insulin from pancreatic β-cells. However, if pancreatic β-cells solely depended on the blood glucose level for insulin secretion, a surge in blood glucose levels would be inevitable after the ingestion of a large amount of carbohydrates. To avoid a deluge of glucose in the bloodstream after a large carbohydrate- rich meal, enteroendocrine cells detect the amount of nutrient absorption from the gut lumen and secrete incretin hormones at scale. Since insulin secretion in response to incretin hormones occurs only in a hyperglycemic milieu, pancreatic β-cells can secrete a “Goldilocks” amount of insulin (i.e., not too much and not too little) to keep the blood glucose level in the normal range. In this regard, pancreatic β-cell sensitivity to glucose and incretin hormones is crucial for maintaining normal glucose homeostasis. In this Namgok lecture 2022, we review the effects of current anti-diabetic medications on pancreatic β-cell sensitivity to glucose and incretin hormones.
-
Citations
Citations to this article as recorded by- Initial Combination Therapy in Type 2 Diabetes
Ji Yoon Kim, Nam Hoon Kim
Endocrinology and Metabolism.2024; 39(1): 23. CrossRef
- Initial Combination Therapy in Type 2 Diabetes

- Miscellaneous
- In Memoriam: Remembering Professor Hun-Ki Min (1928–2021)
- Young Min Cho
- Endocrinol Metab. 2021;36(2):207-208. Published online April 20, 2021
- DOI: https://doi.org/10.3803/EnM.2021.204
- 3,006 View
- 153 Download

- Diabetes
- Peptidyl and Non-Peptidyl Oral Glucagon-Like Peptide-1 Receptor Agonists
- Hun Jee Choe, Young Min Cho
- Endocrinol Metab. 2021;36(1):22-29. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2021.102
- 27,873 View
- 655 Download
- 11 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
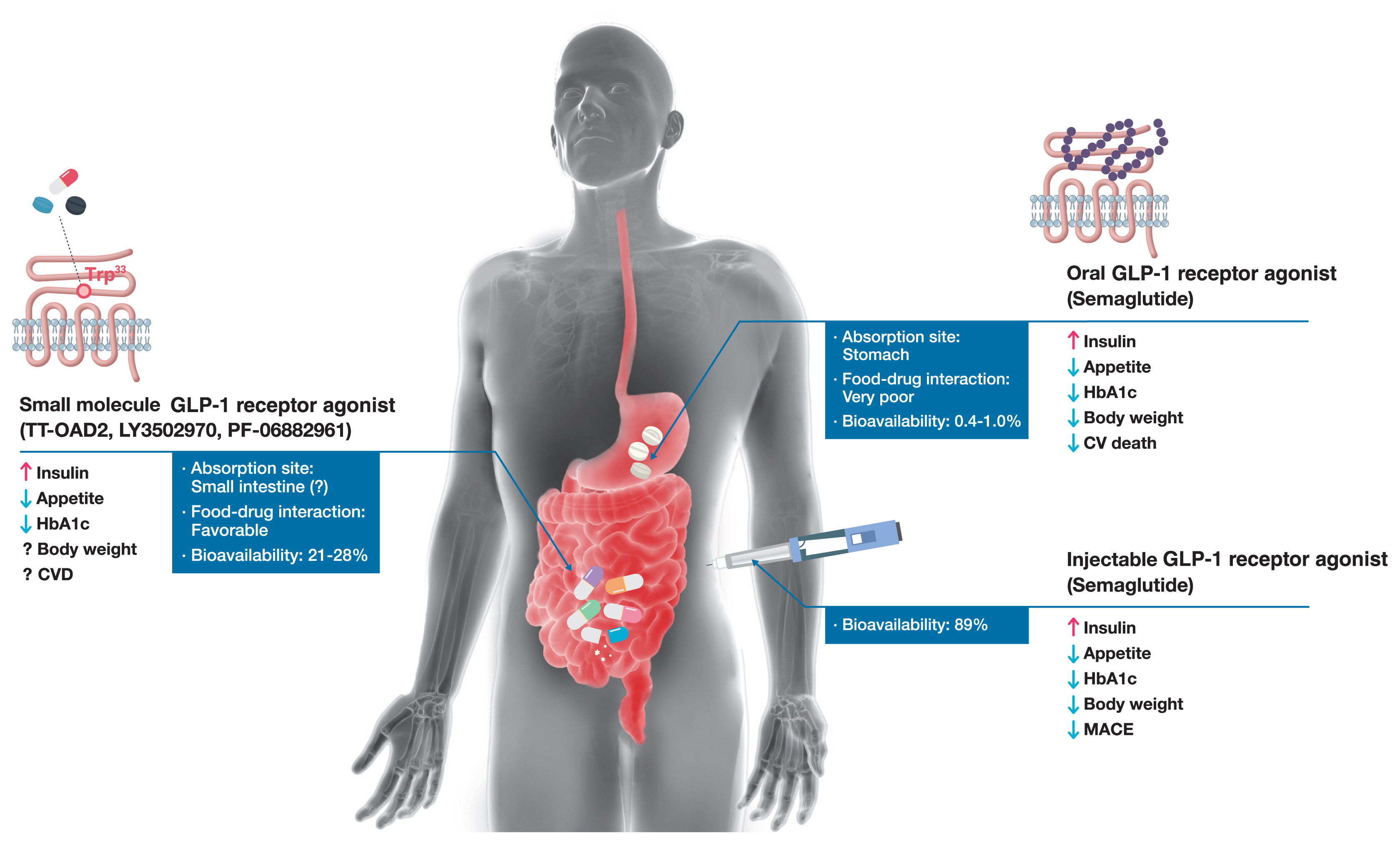
ePub - Glucagon-like peptide-1 (GLP-1) receptor agonists are efficacious glucose-lowering medications with salient benefits for body weight and cardiovascular events. This class of medications is now recommended as the top priority for patients with established cardiovascular disease or indicators of high risk. Until the advent of oral semaglutide, however, GLP-1 receptor agonists were available only in the form of subcutaneous injections. Aversion to needles, discomfort with self-injection, or skin problems at the injection site are commonly voiced problems in people with diabetes, and thus, attempts for non-invasive delivery strategies have continued. Herein, we review the evolution of GLP-1 therapy from its discovery and the development of currently approved drugs to the unprecedented endeavor to administer GLP-1 receptor agonists via the oral route. We focus on the pharmacokinetic and pharmacodynamic properties of the recently approved oral GLP-1 receptor agonist, oral semaglutide. Small molecule oral GLP-1 receptor agonists are currently in development, and we introduce how these chemicals have addressed the challenge posed by interactions with the large extracellular ligand binding domain of the GLP-1 receptor. We specifically discuss the structure and pharmacological properties of TT-OAD2, LY3502970, and PF-06882961, and envision an era where more patients could benefit from oral GLP-1 receptor agonist therapy.
-
Citations
Citations to this article as recorded by- Sulfobetaine modification of poly (D, L-lactide-co-glycolic acid) nanoparticles enhances mucus permeability and improves bioavailability of orally delivered liraglutide
Zhenyu Zhao, Ruihuan Ding, Yumei Wang, Ranran Yuan, Houqian Zhang, Tianyang Li, Wei Zheng, Entao Chen, Aiping Wang, Yanan Shi
Journal of Drug Delivery Science and Technology.2024; 93: 105437. CrossRef - Physiology and pharmacology of glucagon-like peptide-1 receptor
D. V. Kurkin, D. A. Bakulin, E. I. Morkovin, V. I. Petrov, A. V. Strygin, K. N. Koryanova, Yu. V. Gorbunova, Yu. A. Kolosov, O. V. Ivanova, E. V. Pavlova, M. A. Dzhavakhyan, A. V. Zaborovsky, V. B. Saparova, I. E. Makarenko, R. I. Drai, A. N. Chumachenko
Pharmacy & Pharmacology.2024; 11(4): 347. CrossRef - G protein-coupled receptors driven intestinal glucagon-like peptide-1 reprogramming for obesity: Hope or hype?
Mohan Patil, Ilaria Casari, Leon N. Warne, Marco Falasca
Biomedicine & Pharmacotherapy.2024; 172: 116245. CrossRef - Glucagon-like peptide-1 analogs: Miracle drugs are blooming?
Binbin Gong, Zhihong Yao, Chenxu Zhou, Wenxi Wang, Lidan Sun, Jing Han
European Journal of Medicinal Chemistry.2024; 269: 116342. CrossRef - Opportunities and challenges of incretin-based hypoglycemic agents treating type 2 diabetes mellitus from the perspective of physiological disposition
Yaochen Xie, Qian Zhou, Qiaojun He, Xiaoyi Wang, Jincheng Wang
Acta Pharmaceutica Sinica B.2023; 13(6): 2383. CrossRef - Advances in GLP-1 receptor agonists for the treatment of type 2 diabetes
Shurui Hong, J. Xiao, Y. He
BIO Web of Conferences.2023; 61: 01006. CrossRef - Safety and efficacy of the new, oral, small-molecule, GLP-1 receptor agonists orforglipron and danuglipron for the treatment of type 2 diabetes and obesity: systematic review and meta-analysis of randomized controlled trials
Paschalis Karakasis, Dimitrios Patoulias, Konstantinos Pamporis, Panagiotis Stachteas, Konstantinos I. Bougioukas, Aleksandra Klisic, Nikolaos Fragakis, Manfredi Rizzo
Metabolism.2023; 149: 155710. CrossRef - A review of glucoregulatory hormones potentially applicable to the treatment of Alzheimer’s disease: mechanism and brain delivery
Reeju Amatya, Kyoung Ah Min, Meong Cheol Shin
Journal of Pharmaceutical Investigation.2022; 52(2): 195. CrossRef - Anti-Obesity Medications and Investigational Agents: An Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022
Harold E. Bays, Angela Fitch, Sandra Christensen, Karli Burridge, Justin Tondt
Obesity Pillars.2022; 2: 100018. CrossRef - Structural basis of peptidomimetic agonism revealed by small-molecule GLP-1R agonists Boc5 and WB4-24
Zhaotong Cong, Qingtong Zhou, Yang Li, Li-Nan Chen, Zi-Chen Zhang, Anyi Liang, Qing Liu, Xiaoyan Wu, Antao Dai, Tian Xia, Wei Wu, Yan Zhang, Dehua Yang, Ming-Wei Wang
Proceedings of the National Academy of Sciences.2022;[Epub] CrossRef - Improved Split TEV GPCR β-arrestin-2 Recruitment Assays via Systematic Analysis of Signal Peptide and β-arrestin Binding Motif Variants
Yuxin Wu, Isabelle von Hauff, Niels Jensen, Moritz Rossner, Michael Wehr
Biosensors.2022; 13(1): 48. CrossRef - GLP-1 Receptor Agonists: Beyond Their Pancreatic Effects
Xin Zhao, Minghe Wang, Zhitong Wen, Zhihong Lu, Lijuan Cui, Chao Fu, Huan Xue, Yunfeng Liu, Yi Zhang
Frontiers in Endocrinology.2021;[Epub] CrossRef - Recent developments in GLP‐1RA therapy: A review of the latest evidence of efficacy and safety and differences within the class
Evie K. Bain, Stephen C. Bain
Diabetes, Obesity and Metabolism.2021; 23(S3): 30. CrossRef
- Sulfobetaine modification of poly (D, L-lactide-co-glycolic acid) nanoparticles enhances mucus permeability and improves bioavailability of orally delivered liraglutide

- Erratum: Correction of Figure. Clinical Implications of Various Criteria for the Biochemical Diagnosis of Insulinoma
- Chang Ho Ahn, Lee-Kyung Kim, Jie Eun Lee, Chan-Hyeon Jung, Se-Hee Min, Kyong Soo Park, Seong Yeon Kim, Young Min Cho
- Endocrinol Metab. 2017;32(2):306. Published online June 23, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.2.306
- 2,863 View
- 31 Download

- Clinical Study
- 1,5-Anhydro-D-Glucitol Could Reflect Hypoglycemia Risk in Patients with Type 2 Diabetes Receiving Insulin Therapy
- Min Kyeong Kim, Hye Seung Jung, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Seong Yeon Kim
- Endocrinol Metab. 2016;31(2):284-291. Published online May 27, 2016
- DOI: https://doi.org/10.3803/EnM.2016.31.2.284
- 4,376 View
- 41 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The identification of a marker for hypoglycemia could help patients achieve strict glucose control with a lower risk of hypoglycemia. 1,5-Anhydro-D-glucitol (1,5-AG) reflects postprandial hyperglycemia in patients with well-controlled diabetes, which contributes to glycemic variability. Because glycemic variability is related to hypoglycemia, we aimed to evaluate the value of 1,5-AG as a marker of hypoglycemia.
Methods We enrolled 18 adults with type 2 diabetes mellitus (T2DM) receiving insulin therapy and assessed the occurrence of hypoglycemia within a 3-month period. We measured 1,5-AG level, performed a survey to score the severity of hypoglycemia, and applied a continuous glucose monitoring system (CGMS).
Results 1,5-AG was significantly lower in the high hypoglycemia-score group compared to the low-score group. Additionally, the duration of insulin treatment was significantly longer in the high-score group. Subsequent analyses were adjusted by the duration of insulin treatment and mean blood glucose, which was closely associated with both 1,5-AG level and hypoglycemia risk. In adjusted correlation analyses, 1,5-AG was negatively correlated with hypoglycemia score, area under the curve at 80 mg/dL, and low blood glucose index during CGMS (
P =0.068,P =0.033, andP =0.060, respectively).Conclusion 1,5-AG level was negatively associated with hypoglycemia score determined by recall and with documented hypoglycemia after adjusting for mean glucose and duration of insulin treatment. As a result, this level could be a marker of the risk of hypoglycemia in patients with well-controlled T2DM receiving insulin therapy.
-
Citations
Citations to this article as recorded by- Mobile Healthcare System Provided by Primary Care Physicians Improves Quality of Diabetes Care
Tae Jung Oh, Jie-Eun Lee, Seok Kim, Sooyoung Yoo, Hak Chul Jang
CardioMetabolic Syndrome Journal.2021; 1(1): 88. CrossRef - Effects of mobile phone application combined with or without self‐monitoring of blood glucose on glycemic control in patients with diabetes: A randomized controlled trial
Yuan Yu, Qun Yan, Huizhi Li, Hongmei Li, Lin Wang, Hua Wang, Yiyun Zhang, Lei Xu, Zhaosheng Tang, Xinfeng Yan, Yinghua Chen, Huili He, Jie Chen, Bo Feng
Journal of Diabetes Investigation.2019; 10(5): 1365. CrossRef - Articles inEndocrinology and Metabolismin 2016
Won-Young Lee
Endocrinology and Metabolism.2017; 32(1): 62. CrossRef - A Diet Diverse in Bamboo Parts is Important for Giant Panda (Ailuropoda melanoleuca) Metabolism and Health
Hairui Wang, Heju Zhong, Rong Hou, James Ayala, Guangmang Liu, Shibin Yuan, Zheng Yan, Wenping Zhang, Yuliang Liu, Kailai Cai, Zhigang Cai, He Huang, Zhihe Zhang, De Wu
Scientific Reports.2017;[Epub] CrossRef - Low and exacerbated levels of 1,5-anhydroglucitol are associated with cardiovascular events in patients after first-time elective percutaneous coronary intervention
Shuhei Takahashi, Kazunori Shimada, Katsumi Miyauchi, Tetsuro Miyazaki, Eiryu Sai, Manabu Ogita, Shuta Tsuboi, Hiroshi Tamura, Shinya Okazaki, Tomoyuki Shiozawa, Shohei Ouchi, Tatsuro Aikawa, Tomoyasu Kadoguchi, Hamad Al Shahi, Takuma Yoshihara, Makoto Hi
Cardiovascular Diabetology.2016;[Epub] CrossRef
- Mobile Healthcare System Provided by Primary Care Physicians Improves Quality of Diabetes Care

- Clinical Study
- Clinical Characteristics of Subjects with Sulfonylurea-Dependent Type 2 Diabetes
- Se Hee Min, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Hye Seung Jung
- Endocrinol Metab. 2015;30(4):509-513. Published online December 31, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.4.509
- 4,493 View
- 69 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Even though several oral anti-diabetic drugs (OAD) with various modes of action are replacing sulfonylurea (SU), some patients seem to be dependent on SU for adequate glycemic control. Therefore, we evaluated the clinical characteristics of such patients.
Methods We selected the patients with type 2 diabetes who met following criteria from 2009 to 2014 at Seoul National University Hospital: glycated hemoglobin (HbA1c) was maintained below 7.5% for at least 6 months under small dose of SU (glimepiride ≤2 mg/day or equivalent dose); after discontinuation of SU, HbA1c increased ≥1.2% within 3 months or ≥1.5% within 6 months; and after resuming SU, HbA1c reduction was ≥0.8% or reduction of fasting plasma glucose was ≥40 mg/dL within 3 months. Patients with impaired hepatic or renal function, and steroid users were excluded.
Results Nineteen subjects were enrolled: after averaged 4.8±1.5 months of SU-free period, HbA1c increased from 6.7%±0.4% to 8.8%±0.8% even though adding other OAD such as gliptins. However, HbA1c decreased to 7.4%±0.7% after resuming SU within 2.4±0.8 months. There was no sexual predominance. Despite their old age (67±11 years) and long duration of diabetes (18±10 years), fasting C-peptide was relatively well-reserved (3.9±2.6 ng/mL), and nephropathy was not observed (albumin-creatinine ratio 21.2±16.6 mg/g and estimated glomerular filtration rate 75.8±18.0 mL/min/1.73 m2). Strong family history was also noted (73.7%).
Conclusion Despite hypoglycemia risk of SU, it seemed indispensable for a subset of patients with regard to insulin secretion. Genetic influences would be evaluated.
-
Citations
Citations to this article as recorded by- Incident Hepatocellular Carcinoma Risk in Patients Treated with a Sulfonylurea: A Nationwide, Nested, Case-Control Study
Ji-Yeon Lee, Suk-Yong Jang, Chung Mo Nam, Eun Seok Kang
Scientific Reports.2019;[Epub] CrossRef - A genetic variant in GLP1R is associated with response to DPP-4 inhibitors in patients with type 2 diabetes
Eugene Han, Hye Sun Park, Obin Kwon, Eun Yeong Choe, Hye Jin Wang, Yong-ho Lee, Sang-Hak Lee, Chul Hoon Kim, Lee-Kyung Kim, Soo Heon Kwak, Kyong Soo Park, Chul Sik Kim, Eun Seok Kang
Medicine.2016; 95(44): e5155. CrossRef
- Incident Hepatocellular Carcinoma Risk in Patients Treated with a Sulfonylurea: A Nationwide, Nested, Case-Control Study

- Obesity and Metabolism
- Glucagon-Like Peptide-1 Increases Mitochondrial Biogenesis and Function in INS-1 Rat Insulinoma Cells
- Mi Yeon Kang, Tae Jung Oh, Young Min Cho
- Endocrinol Metab. 2015;30(2):216-220. Published online June 30, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.2.216
- 4,013 View
- 44 Download
- 41 Web of Science
- 40 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Glucagon-like peptide-1 (GLP-1) is a gut-derived incretin hormone that increases glucose-stimulated insulin secretion in pancreatic β-cells. Since mitochondrial function is crucial to insulin secretion, we hypothesized that GLP-1 may increase mitochondrial biogenesis in pancreatic β-cells. We treated INS-1 rat insulinoma cells with GLP-1 or exendin-4 for 48 hours and measured mitochondrial mass and function. Both GLP-1 and exendin-4 increased mitochondrial mass by approximately 20%. The mitochondria/cytosol ratio was increased from 7.60±3.12% to 10.53±2.70% by exendin-4. In addition, GLP-1 increased the mitochondrial membrane potential and oxygen consumption. Proliferator-activated receptor-gamma coactivator 1α expression was increased approximately 2-fold by GLP-1 treatment. In conclusion, the present study presents evidence for a new mechanism of action by which GLP-1 improves pancreatic β-cell function via enhanced mitochondrial mass and performance.
-
Citations
Citations to this article as recorded by- New fraternine analogues: Evaluation of the antiparkinsonian effect in the model of Parkinson's disease
Andréia Biolchi Mayer, Henrique de Oliveira Amaral, Danilo Gustavo R. de Oliveira, Gabriel Avohay Alves Campos, Priscilla Galante Ribeiro, Solange Cristina Rego Fernandes, Adolfo Carlos Barros de Souza, Raffael Júnio Araújo de Castro, Anamélia Lorenzetti
Neuropeptides.2024; 103: 102390. CrossRef - Prospects of antidiabetic drugs in the treatment of neurodegenerative disease
Lidan Hu, Wenmin Wang, Xiangjun Chen, Guannan Bai, Liangjian Ma, Xin Yang, Qiang Shu, Xuekun Li
Brain‐X.2024;[Epub] CrossRef - Attenuating mitochondrial dysfunction and morphological disruption with PT320 delays dopamine degeneration in MitoPark mice
Vicki Wang, Kuan-Yin Tseng, Tung-Tai Kuo, Eagle Yi-Kung Huang, Kuo-Lun Lan, Zi-Rong Chen, Kuo-Hsing Ma, Nigel H. Greig, Jin Jung, Ho-II Choi, Lars Olson, Barry J. Hoffer, Yuan-Hao Chen
Journal of Biomedical Science.2024;[Epub] CrossRef - Liraglutide demonstrates a therapeutic effect on mitochondrial dysfunction in human SGBS adipocytes in vitro
Maija Vaittinen, Mariana Ilha, Elena Herbers, Anita Wagner, Kirsi A. Virtanen, Kirsi H. Pietiläinen, Eija Pirinen, Jussi Pihlajamäki
Diabetes Research and Clinical Practice.2023; 199: 110635. CrossRef - The cardioprotective effect of human glucagon‐like peptide‐1 receptor agonist (semaglutide) on cisplatin‐induced cardiotoxicity in rats: Targeting mitochondrial functions, dynamics, biogenesis, and redox status pathways
Marwa Mohamed Atef, Yasser Mostafa Hafez, Omnia Safwat El‐Deeb, Eman H. Basha, Radwa Ismail, Hanan Alshenawy, Rasha Osama El‐Esawy, Amira Kamel Eltokhy
Cell Biochemistry and Function.2023; 41(4): 450. CrossRef - Targeting mitochondrial quality control for diabetic cardiomyopathy: Therapeutic potential of hypoglycemic drugs
Yutong Zhou, Wendong Suo, Xinai Zhang, Jiaojiao Liang, Weizhe Zhao, Yue Wang, Hong Li, Qing Ni
Biomedicine & Pharmacotherapy.2023; 168: 115669. CrossRef - Soft X-ray tomography to map and quantify organelle interactions at the mesoscale
Valentina Loconte, Jitin Singla, Angdi Li, Jian-Hua Chen, Axel Ekman, Gerry McDermott, Andrej Sali, Mark Le Gros, Kate L. White, Carolyn A. Larabell
Structure.2022; 30(4): 510. CrossRef - Comparisons of pleiotropic effects of SGLT2 inhibition and GLP-1 agonism on cardiac glucose intolerance in heart dysfunction
Belma Turan, Aysegul Durak, Yusuf Olgar, Erkan Tuncay
Molecular and Cellular Biochemistry.2022; 477(11): 2609. CrossRef - Modulation of Reactive Oxygen Species Homeostasis as a Pleiotropic Effect of Commonly Used Drugs
Carolin Thomas, Lia Wurzer, Ernst Malle, Michael Ristow, Corina T. Madreiter-Sokolowski
Frontiers in Aging.2022;[Epub] CrossRef - Anti-cancer effects of sitagliptin, vildagliptin, and exendin-4 on triple-negative breast cancer cells via mitochondrial modulation
POOJA JAISWAL, VERSHA TRIPATHI, ANSHUL ASSAIYA, DHARMENDRA KASHYAP, RAHUL DUBEY, ANAMIKA SINGH, JANESH KUMAR, HEM CHANDRA JHA, RAJESH SHARMA, AMIT KUMAR DIXIT, HAMENDRA SINGH PARMAR
BIOCELL.2022; 46(12): 2645. CrossRef - Effect of liraglutide on neural and peripheral markers of metabolic function during antipsychotic treatment in rats
Ilijana Babic, Dominic Sellers, Paul L Else, Jessica Nealon, Ashleigh L Osborne, Nagesh Pai, Katrina Weston-Green
Journal of Psychopharmacology.2021; 35(3): 284. CrossRef - Sustained Release GLP-1 Agonist PT320 Delays Disease Progression in a Mouse Model of Parkinson’s Disease
Vicki Wang, Tung-Tai Kuo, Eagle Yi-Kung Huang, Kuo-Hsing Ma, Yu-Ching Chou, Zhao-Yang Fu, Li-Wen Lai, Jin Jung, Hoi-II Choi, Doo-Sup Choi, Yazhou Li, Lars Olson, Nigel H. Greig, Barry J. Hoffer, Yuan-Hao Chen
ACS Pharmacology & Translational Science.2021; 4(2): 858. CrossRef - Antioxidative Potentials of Incretin-Based Medications: A Review of Molecular Mechanisms
Habib Yaribeygi, Mina Maleki, Thozhukat Sathyapalan, Tannaz Jamialahmadi, Amirhossein Sahebkar, Marina Sokovi
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - Vernicia fordii (Hemsl.) Airy Shaw extract stimulates insulin secretion in pancreatic β-cells and improves insulin sensitivity in diabetic mice
Jimin Hyun, Mi Hyeon Park, Yo Han Lee, Youngeun Lee, Su Ji Jeong, Sun Sil Choi, Keon Woo Khim, Hye Jin Eom, Jin-Hoe Hur, Chan Young Park, Jae-Ick Kim, Jiyoung Park, Hyung Won Ryu, Hyun-Jun Jang, Sei-Ryang Oh, Jang Hyun Choi
Journal of Ethnopharmacology.2021; 278: 114238. CrossRef - Connecting the dots between mitochondrial dysfunction and Parkinson’s disorder: focus mitochondria-targeting therapeutic paradigm in mitigating the disease severity
Ishnoor Kaur, Tapan Behl, Aayush Sehgal, Sukhbir Singh, Neelam Sharma, Lotfi Aleya, Simona Bungau
Environmental Science and Pollution Research.2021; 28(28): 37060. CrossRef - Neuromodulatory effects of anti-diabetes medications: A mechanistic review
Habib Yaribeygi, Milad Ashrafizadeh, Neil C. Henney, Thozhukat Sathyapalan, Tannaz Jamialahmadi, Amirhossein Sahebkar
Pharmacological Research.2020; 152: 104611. CrossRef - Antidiabetic Agents for Treatment of Parkinson’s Disease: A Meta-Analysis
Shu-Yi Wang, Shey-Lin Wu, Ta-Cheng Chen, Chieh-Sen Chuang
International Journal of Environmental Research and Public Health.2020; 17(13): 4805. CrossRef - Visualizing subcellular rearrangements in intact β cells using soft x-ray tomography
Kate L. White, Jitin Singla, Valentina Loconte, Jian-Hua Chen, Axel Ekman, Liping Sun, Xianjun Zhang, John Paul Francis, Angdi Li, Wen Lin, Kaylee Tseng, Gerry McDermott, Frank Alber, Andrej Sali, Carolyn Larabell, Raymond C. Stevens
Science Advances.2020;[Epub] CrossRef - Nutrient Sensor mTOR and OGT: Orchestrators of Organelle Homeostasis in Pancreatic β-Cells
Nicholas Esch, Seokwon Jo, Mackenzie Moore, Emilyn U. Alejandro, Yingke Xu
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Metabolic dynamics of human Sertoli cells are differentially modulated by physiological and pharmacological concentrations of GLP-1
Ana D. Martins, Mariana P. Monteiro, Branca M. Silva, Alberto Barros, Mário Sousa, Rui A. Carvalho, Pedro F. Oliveira, Marco G. Alves
Toxicology and Applied Pharmacology.2019; 362: 1. CrossRef - Sarcopenia in Chronic Kidney Disease: Factors, Mechanisms, and Therapeutic Interventions
Hiroshi Watanabe, Yuki Enoki, Toru Maruyama
Biological and Pharmaceutical Bulletin.2019; 42(9): 1437. CrossRef - Recent Advances in Drug Repurposing for Parkinson’s Disease
Xin Chen, Giuseppe Gumina, Kristopher G. Virga
Current Medicinal Chemistry.2019; 26(28): 5340. CrossRef - Mitochondrial dysfunction in diabetes and the regulatory roles of antidiabetic agents on the mitochondrial function
Habib Yaribeygi, Stephen L. Atkin, Amirhossein Sahebkar
Journal of Cellular Physiology.2019; 234(6): 8402. CrossRef - Liraglutide protects against glucolipotoxicity‐induced RIN‐m5F β‐cell apoptosis through restoration of PDX1 expression
Edy Kornelius, Hsin‐Hua Li, Chiung‐Huei Peng, Yi‐Sun Yang, Wei‐Jen Chen, Yan‐Zin Chang, Yi‐Chiao Bai, Stanley Liu, Chien‐Ning Huang, Chih‐Li Lin
Journal of Cellular and Molecular Medicine.2019; 23(1): 619. CrossRef - The osteogenic effect of liraglutide involves enhanced mitochondrial biogenesis in osteoblasts
Subhashis Pal, Shailendra K. Maurya, Sourav Chattopadhyay, Shyamsundar Pal China, Konica Porwal, Chirag Kulkarni, Sabyasachi Sanyal, Rohit A. Sinha, Naibedya Chattopadhyay
Biochemical Pharmacology.2019; 164: 34. CrossRef - Novel Treatment Opportunities Against Cognitive Impairment in Parkinson’s Disease with an Emphasis on Diabetes-Related Pathways
Holly Green, Panagiota Tsitsi, Ioanna Markaki, Dag Aarsland, Per Svenningsson
CNS Drugs.2019; 33(2): 143. CrossRef - Mitral cells and the glucagon‐like peptide 1 receptor: The sweet smell of success?
Enrico Bagnoli, Una FitzGerald
European Journal of Neuroscience.2019; 49(4): 422. CrossRef - Targeting the DPP-4-GLP-1 pathway improves exercise tolerance in heart failure patients: a systematic review and meta-analysis
Chengcong Chen, Ying Huang, Yongmei Zeng, Xiyan Lu, Guoqing Dong
BMC Cardiovascular Disorders.2019;[Epub] CrossRef - Acute exposure to 3‑deoxyglucosone at high glucose levels impairs insulin secretion from β‑cells by downregulating the sweet taste receptor signaling pathway
Xiudao Song, Guoqiang Liang, Min Shi, Liang Zhou, Fei Wang, Lurong Zhang, Fei Huang, Guorong Jiang
Molecular Medicine Reports.2019;[Epub] CrossRef - Translational approaches to restoring mitochondrial function in Parkinson's disease
Heather Mortiboys, Ruby Macdonald, Thomas Payne, Matilde Sassani, Thomas Jenkins, Oliver Bandmann
FEBS Letters.2018; 592(5): 776. CrossRef - Neuroprotective exendin-4 enhances hypothermia therapy in a model of hypoxic-ischaemic encephalopathy
Eridan Rocha-Ferreira, Laura Poupon, Aura Zelco, Anna-Lena Leverin, Syam Nair, Andrea Jonsdotter, Ylva Carlsson, Claire Thornton, Henrik Hagberg, Ahad A Rahim
Brain.2018; 141(10): 2925. CrossRef - Current perspective of mitochondrial biology in Parkinson's disease
Navneet Ammal Kaidery, Bobby Thomas
Neurochemistry International.2018; 117: 91. CrossRef - Humanin promotes mitochondrial biogenesis in pancreatic MIN6 β-cells
Qingqing Qin, Jieqiong Jin, Fang He, Yongqin Zheng, Tingting Li, Yun Zhang, Jundong He
Biochemical and Biophysical Research Communications.2018; 497(1): 292. CrossRef - Exenatide once weekly versus placebo in Parkinson's disease: a randomised, double-blind, placebo-controlled trial
Dilan Athauda, Kate Maclagan, Simon S Skene, Martha Bajwa-Joseph, Dawn Letchford, Kashfia Chowdhury, Steve Hibbert, Natalia Budnik, Luca Zampedri, John Dickson, Yazhou Li, Iciar Aviles-Olmos, Thomas T Warner, Patricia Limousin, Andrew J Lees, Nigel H Grei
The Lancet.2017; 390(10103): 1664. CrossRef - Alogliptin, a Dipeptidyl Peptidase‐4 Inhibitor, Alleviates Atrial Remodeling and Improves Mitochondrial Function and Biogenesis in Diabetic Rabbits
Xiaowei Zhang, Zhiwei Zhang, Yungang Zhao, Ning Jiang, Jiuchun Qiu, Yajuan Yang, Jian Li, Xue Liang, Xinghua Wang, Gary Tse, Guangping Li, Tong Liu
Journal of the American Heart Association.2017;[Epub] CrossRef - Potential therapeutic interventions for chronic kidney disease‐associated sarcopenia via indoxyl sulfate‐induced mitochondrial dysfunction
Yuki Enoki, Hiroshi Watanabe, Riho Arake, Rui Fujimura, Kana Ishiodori, Tadashi Imafuku, Kento Nishida, Ryusei Sugimoto, Saori Nagao, Shigeyuki Miyamura, Yu Ishima, Motoko Tanaka, Kazutaka Matsushita, Hirotaka Komaba, Masafumi Fukagawa, Masaki Otagiri, To
Journal of Cachexia, Sarcopenia and Muscle.2017; 8(5): 735. CrossRef - The pancreas: Bandmaster of glucose homeostasis
Nathalie Jouvet, Jennifer L. Estall
Experimental Cell Research.2017; 360(1): 19. CrossRef - The glucagon-like peptide 1 (GLP) receptor as a therapeutic target in Parkinson's disease: mechanisms of action
Dilan Athauda, Thomas Foltynie
Drug Discovery Today.2016; 21(5): 802. CrossRef - Effects of addition of a dipeptidyl peptidase IV inhibitor to metformin on sirolimus-induced diabetes mellitus
Long Jin, Sun Woo Lim, Jian Jin, Byung Ha Chung, Chul Woo Yang
Translational Research.2016; 174: 122. CrossRef - Pharmacological Modulators of Endoplasmic Reticulum Stress in Metabolic Diseases
Tae Jung, Kyung Choi
International Journal of Molecular Sciences.2016; 17(2): 192. CrossRef
- New fraternine analogues: Evaluation of the antiparkinsonian effect in the model of Parkinson's disease

- Obesity and Metabolism
- Mitochondrial Complexes I and II Are More Susceptible to Autophagy Deficiency in Mouse β-Cells
- Min Joo Kim, Ok Kyong Choi, Kyung Sil Chae, Min Kyeong Kim, Jung Hee Kim, Masaaki Komatsu, Keiji Tanaka, Hakmo Lee, Sung Soo Chung, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, Hye Seung Jung
- Endocrinol Metab. 2015;30(1):65-70. Published online March 27, 2015
- DOI: https://doi.org/10.3803/EnM.2015.30.1.65
- 3,956 View
- 40 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Damaged mitochondria are removed by autophagy. Therefore, impairment of autophagy induces the accumulation of damaged mitochondria and mitochondrial dysfunction in most mammalian cells. Here, we investigated mitochondrial function and the expression of mitochondrial complexes in autophagy-related 7 (
Atg7 )-deficient β-cells.Methods To evaluate the effect of autophagy deficiency on mitochondrial function in pancreatic β-cells, we isolated islets from
Atg7 F/F:RIP-Cre + mice and wild-type littermates. Oxygen consumption rate and intracellular adenosine 5'-triphosphate (ATP) content were measured. The expression of mitochondrial complex genes inAtg7 -deficient islets and in β-TC6 cells transfected with siAtg7 was measured by quantitative real-time polymerase chain reaction.Results Baseline oxygen consumption rate of
Atg7 -deficient islets was significantly lower than that of control islets (P <0.05). Intracellular ATP content ofAtg7 -deficient islets during glucose stimulation was also significantly lower than that of control islets (P <0.05). By Oxygraph-2k analysis, mitochondrial respiration inAtg7 -deficient islets was significantly decreased overall, although state 3 respiration and responses to antimycin A were unaffected. The mRNA levels of mitochondrial complexes I, II, III, and V inAtg7 -deficient islets were significantly lower than in control islets (P <0.05). Down-regulation ofAtg7 in β-TC6 cells also reduced the expression of complexes I and II, with marginal significance (P <0.1).Conclusion Impairment of autophagy in pancreatic β-cells suppressed the expression of some mitochondrial respiratory complexes, and may contribute to mitochondrial dysfunction. Among the complexes, I and II seem to be most vulnerable to autophagy deficiency.
-
Citations
Citations to this article as recorded by- Proteomic pathways to metabolic disease and type 2 diabetes in the pancreatic islet
Belinda Yau, Sheyda Naghiloo, Alexis Diaz-Vegas, Austin V. Carr, Julian Van Gerwen, Elise J. Needham, Dillon Jevon, Sing-Young Chen, Kyle L. Hoehn, Amanda E. Brandon, Laurence Macia, Gregory J. Cooney, Michael R. Shortreed, Lloyd M. Smith, Mark P. Keller,
iScience.2021; 24(10): 103099. CrossRef - Natural compound oblongifolin C inhibits autophagic flux, and induces apoptosis and mitochondrial dysfunction in human cholangiocarcinoma QBC939 cells
Aiqing Zhang, Wei He, Huimin Shi, Xiaodan Huang, Guozhong Ji
Molecular Medicine Reports.2016; 14(4): 3179. CrossRef - Autophagy deficiency in β cells blunts incretin-induced suppression of glucagon release from α cells
Min Joo Kim, Ok Kyong Choi, Kyung Sil Chae, Hakmo Lee, Sung Soo Chung, Dong-Sik Ham, Ji-Won Kim, Kun-Ho Yoon, Kyong Soo Park, Hye Seung Jung
Islets.2015; 7(5): e1129096. CrossRef
- Proteomic pathways to metabolic disease and type 2 diabetes in the pancreatic islet

- Obesity and Metabolism
- Clinical Implications of Various Criteria for the Biochemical Diagnosis of Insulinoma
- Chang Ho Ahn, Lee-Kyung Kim, Jie Eun Lee, Chan-Hyeon Jung, Se-Hee Min, Kyong Soo Park, Seong Yeon Kim, Young Min Cho
- Endocrinol Metab. 2014;29(4):498-504. Published online December 29, 2014
- DOI: https://doi.org/10.3803/EnM.2014.29.4.498
- 4,420 View
- 74 Download
- 10 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Among the various diagnostic criteria for insulinoma, the ratio criteria have been controversial. However, the amended insulin-glucose ratio exhibited excellent diagnostic performance in a recent retrospective cohort study, although it has not yet been validated in other patient cohorts. We examined the diagnostic performance of the current criteria of the Endocrine Society, insulin-glucose ratio, C-peptide-glucose ratio, and amended ratios in terms of differentiating insulinomas.
Methods We reviewed the medical records of patients who underwent evaluation for hypoglycemia from 2000 to 2013. Fourteen patients with histopathologically confirmed insulinoma and 18 patients without clinical evidence of insulinoma were included. The results of a prolonged fast test were analyzed according to the abovementioned criteria.
Results Fulfilling all three Endocrine Society criteria-plasma levels of glucose (<3.0 mmol/L), insulin (≥8 pmol/L), and C-peptide (≥0.2 nmol/L)-exhibited 100% sensitivity and 89% specificity. Fulfilling the glucose and C-peptide criteria showed 100% sensitivity and 83% specificity, while fulfilling the glucose and insulin criteria showed 100% sensitivity and 72% specificity. Among the ratio criteria, the insulin-glucose ratio [>24.0 (pmol/L)/(mmol/L)] gave the highest area under the receiver operating characteristic curve, with 93% sensitivity and 94% specificity.
Conclusion Fulfilling the glucose, insulin, and C-peptide criteria of the Endocrine Society guidelines exhibited the best diagnostic performance for insulinoma. Nonetheless, the insulin-glucose ratio may still have a role in the biochemical diagnosis of insulinoma.
-
Citations
Citations to this article as recorded by- Homeostasis Model Assessment of β-Cell Function for Diagnosis of Insulinoma
Kálmán Bódis, Martin Schön, Laura Dauben, Miriam Wilker, Klaus Strassburger, Volker Burkart, Michael Roden, Karsten Müssig
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1125. CrossRef - A novel diagnostic model for insulinoma
Feng Wang, Zhe Yang, XiuBing Chen, Yiling Peng, HaiXing Jiang, ShanYu Qin
Discover Oncology.2022;[Epub] CrossRef - Comparison of the diagnostic accuracy of the current guidelines for detecting insulinoma
Laura Dauben, Marie-Christine Simon, Klaus Strassburger, Volker Burkart, Katharina S Weber, Sven Schinner, Michael Roden, Karsten Müssig
European Journal of Endocrinology.2019; 180(6): 381. CrossRef - EUS-guided lauromacrogol ablation of insulinomas: a novel treatment
Shanyu Qin, Yongru Liu, Hongjian Ning, Lin Tao, Wei Luo, Donghong Lu, Zuojie Luo, Yingfen Qin, Jia Zhou, Junqiang Chen, Haixing Jiang
Scandinavian Journal of Gastroenterology.2018; 53(5): 616. CrossRef - Diagnosis of insulinoma using the ratios of serum concentrations of insulin and C-peptide to glucose during a 5-hour oral glucose tolerance test
Xu Li, Feng Zhang, Haibing Chen, Haoyong Yu, Jian Zhou, Ming Li, Qing Li, Lianxi Li, Jun Yin, Fang Liu, Yuqian Bao, Junfeng Han, Weiping Jia
Endocrine Journal.2017; 64(1): 49. CrossRef - Insulinoma in a 5‐Year‐Old Dexter Cow
C. Binici, S. Plog, O. Kershaw, M. Schmicke, J.H. van der Kolk, K.E. Müller
Journal of Veterinary Internal Medicine.2016; 30(4): 1402. CrossRef - Vague neuroglycopenic complaints camouflage diagnosis of adolescent insulinoma: a case report
Kelsee Halpin, Ryan McDonough, Patria Alba, Jared Halpin, Vivekanand Singh, Yun Yan
International Journal of Pediatric Endocrinology.2016;[Epub] CrossRef - Articles in 'Endocrinology and Metabolism' in 2014
Won-Young Lee
Endocrinology and Metabolism.2015; 30(1): 47. CrossRef
- Homeostasis Model Assessment of β-Cell Function for Diagnosis of Insulinoma

- Obesity and Metabolism
- A Novel Mutation in the Von Hippel-Lindau Tumor Suppressor Gene Identified in a Patient Presenting with Gestational Diabetes Mellitus
- Yun Hyi Ku, Chang Ho Ahn, Chan-Hyeon Jung, Jie Eun Lee, Lee-Kyung Kim, Soo Heon Kwak, Hye Seung Jung, Kyong Soo Park, Young Min Cho
- Endocrinol Metab. 2013;28(4):320-325. Published online December 12, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.4.320
- 3,563 View
- 29 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Von Hippel-Lindau (VHL) disease is an autosomal dominantly inherited, multisystemic tumor syndrome caused by mutations in the
VHL gene. To date, more than 1,000 germline and somatic mutations of theVHL gene have been reported. We present a novel mutation in theVHL tumor suppressor gene that presented with gestational diabetes mellitus.Methods A 30-year-old woman presented with gestational diabetes mellitus. She sequentially showed multiple pancreatic cysts, spinal cord hemangioblastoma, cerebellar hemangioblastoma, and clear cell type renal cell carcinomas. Also, her father and brother had brain hemangioblastomas. Each of the three exons of the
VHL gene was individually amplified by polymerase chain reaction and direct sequencing was performed using an ABI 3730 DNA analyzer.Results DNA sequence analysis to determine the presence of
VHL mutation in her family revealed del291C, a novel frameshift mutation.Conclusion We found a novel mutation in the
VHL tumor suppressor gene that presented with gestational diabetes mellitus.-
Citations
Citations to this article as recorded by- Diversities of Mechanism in Patients with VHL Syndrome and diabetes: A Report of Two Cases and Literature Review
Yanlei Wang, Zhaoxiang Liu, Wenhui Zhao, Chenxiang Cao, Luqi Xiao, Jianzhong Xiao
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 1611. CrossRef - Retinal hemangioblastoma in a patient with Von Hippel-Lindau disease: A case report and literature review
Yikeng Huang, Weiwen Hu, Xionggao Huang
Frontiers in Oncology.2022;[Epub] CrossRef - Updates on the Role of Molecular Alterations and NOTCH Signalling in the Development of Neuroendocrine Neoplasms
Claudia von Arx, Monica Capozzi, Elena López-Jiménez, Alessandro Ottaiano, Fabiana Tatangelo, Annabella Di Mauro, Guglielmo Nasti, Maria Lina Tornesello, Salvatore Tafuto
Journal of Clinical Medicine.2019; 8(9): 1277. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Diversities of Mechanism in Patients with VHL Syndrome and diabetes: A Report of Two Cases and Literature Review

- Obesity and Metabolism
- Clinical Application of Glucagon-Like Peptide 1 Receptor Agonists for the Treatment of Type 2 Diabetes Mellitus
- Young Min Cho, Rhonda D. Wideman, Timothy J. Kieffer
- Endocrinol Metab. 2013;28(4):262-274. Published online December 12, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.4.262
- 5,309 View
- 82 Download
- 37 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Glucagon-like peptide 1 (GLP-1) is secreted from enteroendocrine L-cells in response to oral nutrient intake and elicits glucose-stimulated insulin secretion while suppressing glucagon secretion. It also slows gastric emptying, which contributes to decreased postprandial glycemic excursions. In the 1990s, chronic subcutaneous infusion of GLP-1 was found to lower blood glucose levels in patients with type 2 diabetes. However, GLP-1's very short half-life, arising from cleavage by the enzyme dipeptidyl peptidase 4 (DPP-4) and glomerular filtration by the kidneys, presented challenges for clinical use. Hence, DPP-4 inhibitors were developed, as well as several GLP-1 analogs engineered to circumvent DPP-4-mediated breakdown and/or rapid renal elimination. Three categories of GLP-1 analogs, are being developed and/or are in clinical use: short-acting, long-acting, and prolonged-acting GLP-1 analogs. Each class has different plasma half-lives, molecular size, and homology to native GLP-1, and consequently different characteristic effects on glucose metabolism. In this article, we review current clinical data derived from each class of GLP-1 analogs, and consider the clinical effects reported for each category in recent head to head comparison studies. Given the relatively brief clinical history of these compounds, we also highlight several important efficacy and safety issues which will require further investigation.
-
Citations
Citations to this article as recorded by- The efficacy and safety of combined GLP-1RA and basal insulin therapy among inadequately controlled T2D with premixed insulin therapy
Jhih-Syuan Liu, Sheng-Chiang Su, Feng-Chih Kuo, Peng-Fei Li, Chia-Luen Huang, Li-Ju Ho, Kuan-Chan Chen, Yi-Chen Liu, Chih-Ping Lin, An-Che Cheng, Chien-Hsing Lee, Fu-Huang Lin, Yi-Jen Hung, Hsin-Ya Liu, Chieh-Hua Lu, Chang-Hsun Hsieh
Medicine.2023; 102(10): e33167. CrossRef - Pharmacogenetics of Glucagon-like-peptide-1 receptor in diabetes management
Mariya Kalinkova, Tanya Kadiyska, Teodora Handjieva-Darlenska
Pharmacia.2023; 70(2): 383. CrossRef - Anti-inflammatory potential of liraglutide, a glucagon-like peptide-1 receptor agonist, in rats with peripheral acute inflammation
Irem Mert, Ayhan Cetinkaya, Mujgan Gurler, Canan Akünal Turel, Humeyra Celik, Ibrahim Ethem Torun, Idris Turel
Inflammopharmacology.2022; 30(3): 1093. CrossRef - Exenatide improves hepatocyte insulin resistance induced by different regional adipose tissue
Chuanmin Bai, Yujun Wang, Zhi Niu, Yaxin Guan, Jingshan Huang, Xin Nian, Fan Zuo, Juan Zhao, Tsutomu Kazumi, Bin Wu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Peptidyl and Non-Peptidyl Oral Glucagon-Like Peptide-1 Receptor Agonists
Hun Jee Choe, Young Min Cho
Endocrinology and Metabolism.2021; 36(1): 22. CrossRef - Glucagon-like Peptide-1 Improves Fatty Liver and Enhances Thermogenesis in Brown Adipose Tissue via Inhibiting BMP4-Related Signaling Pathway in High-Fat-Diet-Induced Obese Mice
Xingchun Wang, Bingwei Ma, Jiaqi Chen, Hui You, Chunjun Sheng, Peng Yang, Shen Qu, Vito Angelo Giagulli
International Journal of Endocrinology.2021; 2021: 1. CrossRef - Exenatide ameliorates experimental non-alcoholic fatty liver in rats via suppression of toll-like receptor 4/NFκB signaling: Comparison to metformin
Zeinab A. Saad, Dina M. Khodeer, Sawsan A. Zaitone, Amal A.M. Ahmed, Yasser M. Moustafa
Life Sciences.2020; 253: 117725. CrossRef - Exenatide ameliorates hepatic steatosis and attenuates fat mass and FTO gene expression through PI3K signaling pathway in nonalcoholic fatty liver disease
Shan Li, Xiaoman Wang, Jielei Zhang, Jingyi Li, Xiaogang Liu, Yuanyuan Ma, Chao Han, Lixia Zhang, Lili Zheng
Brazilian Journal of Medical and Biological Research.2018;[Epub] CrossRef - Efficacy and safety of combination therapy with an α‐glucosidase inhibitor and a dipeptidyl peptidase‐4 inhibitor in patients with type 2 diabetes mellitus: A systematic review with meta‐analysis
Se Hee Min, Jeong‐Hwa Yoon, Seokyung Hahn, Young Min Cho
Journal of Diabetes Investigation.2018; 9(4): 893. CrossRef - Glucagon-like peptide-1 affects human umbilical vein endothelial cells in high glucose by the PI3K/Akt/eNOS signaling pathway
Jie Wu, Pingfan Guo, Tianmin He, Fanggang Cai
Turkish Journal of Biochemistry.2018; 43(2): 119. CrossRef - What next after basal insulin? Treatment intensification with lixisenatide in Asian patients with type 2 diabetes mellitus
Wing B. Chan, Andrea Luk, Wing S. Chow, Vincent T.F. Yeung
Journal of Diabetes.2017; 9(6): 562. CrossRef - Treatment potential of the GLP-1 receptor agonists in type 2 diabetes mellitus: a review
L. Østergaard, Christian S. Frandsen, S. Madsbad
Expert Review of Clinical Pharmacology.2016; 9(2): 241. CrossRef - Efficacy and safety of dulaglutide in the treatment of type 2 diabetes: a comprehensive review of the dulaglutide clinical data focusing on the AWARD phase 3 clinical trial program
Johan Jendle, George Grunberger, Thomas Blevins, Francesco Giorgino, Ryan T. Hietpas, Fady T. Botros
Diabetes/Metabolism Research and Reviews.2016; 32(8): 776. CrossRef - Glucagon‐like peptide‐1(GLP‐1) receptor agonists: potential to reduce fracture risk in diabetic patients?
Guojing Luo, Hong Liu, Hongyun Lu
British Journal of Clinical Pharmacology.2016; 81(1): 78. CrossRef - Impact of postprandial glucose control on diabetes-related complications: How is the evidence evolving?
Sten Madsbad
Journal of Diabetes and its Complications.2016; 30(2): 374. CrossRef - Risk assessment and management of post-transplant diabetes mellitus
Eugene Han, Myoung Soo Kim, Yu Seun Kim, Eun Seok Kang
Metabolism.2016; 65(10): 1559. CrossRef - Recent advances in oral delivery of peptide hormones
Pegah Varamini, Istvan Toth
Expert Opinion on Drug Delivery.2016; 13(4): 507. CrossRef - Exendin-4 Inhibits Hepatic Lipogenesis by Increasing β-Catenin Signaling
Mi Hae Seo, Jinmi Lee, Seok-Woo Hong, Eun-Jung Rhee, Se Eun Park, Cheol Young Park, Ki Won Oh, Sung Woo Park, Won-Young Lee, Catherine Mounier
PLOS ONE.2016; 11(12): e0166913. CrossRef - Review of head‐to‐head comparisons of glucagon‐like peptide‐1 receptor agonists
Sten Madsbad
Diabetes, Obesity and Metabolism.2016; 18(4): 317. CrossRef - Does Bosentan Protect Diabetic Brain Alterations in Rats? The Role of Endothelin‐1 in the Diabetic Brain
Recep Demir, Elif Cadirci, Erol Akpinar, Yasemin Cayir, Hasan Tarik Atmaca, Harun Un, Celalettin Semih Kunak, Muhammed Yayla, Zafer Bayraktutan, Ilknur Demir
Basic & Clinical Pharmacology & Toxicology.2015; 116(3): 236. CrossRef - Efficacy and tolerability of albiglutide versus placebo or pioglitazone over 1 year in people with type 2 diabetes currently taking metformin and glimepiride: HARMONY 5
P. D. Home, P. Shamanna, M. Stewart, F. Yang, M. Miller, C. Perry, M. C. Carr
Diabetes, Obesity and Metabolism.2015; 17(2): 179. CrossRef - Differential effects of prandial and non-prandial GLP-1 receptor agonists in type 2 diabetes therapy
Jaime A. Davidson
Postgraduate Medicine.2015; 127(8): 827. CrossRef - GLP‐1 receptor agonists: effects on the progression of non‐alcoholic fatty liver disease
Jia Liu, Guang Wang, Yumei Jia, Yuan Xu
Diabetes/Metabolism Research and Reviews.2015; 31(4): 329. CrossRef - Efficacy and safety of teneligliptin, a dipeptidyl peptidase‐4 inhibitor, combined with metformin in Korean patients with type 2 diabetes mellitus: a 16‐week, randomized, double‐blind, placebo‐controlled phase III trial
M. K. Kim, E.‐J. Rhee, K. A. Han, A. C. Woo, M.‐K. Lee, B. J. Ku, C. H. Chung, K.‐A. Kim, H. W. Lee, I. B. Park, J. Y. Park, H. C. Chul Jang, K. S. Park, W. I. Jang, B. Y. Cha
Diabetes, Obesity and Metabolism.2015; 17(3): 309. CrossRef - Incretin physiology and pathophysiology from an Asian perspective
Young Min Cho
Journal of Diabetes Investigation.2015; 6(5): 495. CrossRef - Response: Economic Impact of Combining Metformin with Dipeptidyl Peptidase-4 Inhibitors in Diabetic Patients with Renal Impairment in Spanish Patients (Diabetes Metab J2015;39:74-81)
Antoni Sicras-Mainar, Ruth Navarro-Artieda
Diabetes & Metabolism Journal.2015; 39(2): 173. CrossRef - Clinical Application of Glucagon-Like Peptide-1 Receptor Agonists
Se Hee Min, Young Min Cho
The Journal of Korean Diabetes.2015; 16(4): 252. CrossRef - Autophagy deficiency in β cells blunts incretin-induced suppression of glucagon release from α cells
Min Joo Kim, Ok Kyong Choi, Kyung Sil Chae, Hakmo Lee, Sung Soo Chung, Dong-Sik Ham, Ji-Won Kim, Kun-Ho Yoon, Kyong Soo Park, Hye Seung Jung
Islets.2015; 7(5): e1129096. CrossRef - Glucagon-Like Peptide-1 Increases Mitochondrial Biogenesis and Function in INS-1 Rat Insulinoma Cells
Mi Yeon Kang, Tae Jung Oh, Young Min Cho
Endocrinology and Metabolism.2015; 30(2): 216. CrossRef - Interleukin-6 CpG Methylation and Body Weight Correlate Differently in Type 2 Diabetes Patients Compared to Obese and Lean Controls
Eva Aumueller, Marlene Remely, Hanna Baeck, Berit Hippe, Helmut Brath, Alexander G. Haslberger
Lifestyle Genomics.2015; 8(1): 26. CrossRef - The glucagon-like peptide 1 receptor agonist enhances intrinsic peroxisome proliferator-activated receptor γ activity in endothelial cells
Hirohisa Onuma, Kouichi Inukai, Atsuko Kitahara, Rie Moriya, Susumu Nishida, Toshiaki Tanaka, Hidenori Katsuta, Kazuto Takahashi, Yoshikazu Sumitani, Toshio Hosaka, Hitoshi Ishida
Biochemical and Biophysical Research Communications.2014; 451(2): 339. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef - Cytokines and Hormones That Contribute to the Positive Association between Fat and Bone
Dorit Naot, Jillian Cornish
Frontiers in Endocrinology.2014;[Epub] CrossRef - Study of Postprandial Lipaemia in Type 2 Diabetes Mellitus: Exenatide versus Liraglutide
Maria Voukali, Irene Kastrinelli, Sapfo Stragalinou, Dimitra Tasiopoulou, Pinelopi Paraskevopoulou, Nicholas Katsilambros, Alexandros Kokkinos, Nicholas Tentolouris, Ioannis Ioannidis
Journal of Diabetes Research.2014; 2014: 1. CrossRef - The cardiometabolic benefits of glycine: Is glycine an ‘antidote’ to dietary fructose?
Mark F McCarty, James J DiNicolantonio
Open Heart.2014; 1(1): e000103. CrossRef - Nuevos fármacos antidiabéticos: avanzando hacia el control integral de la diabesidad
J.J. Gorgojo-Martínez
Hipertensión y Riesgo Vascular.2014; 31(2): 45. CrossRef - Managing Loss of Glycemic Control in Middle-Aged Patients With Diabetes: The Role of GLP-1 Receptor Agonists in Combination-Therapy Regimens
Thomas B. Repas
Journal of Osteopathic Medicine.2014; 114(s52): 14. CrossRef
- The efficacy and safety of combined GLP-1RA and basal insulin therapy among inadequately controlled T2D with premixed insulin therapy

- Obesity and Metabolism
- Hemoglobin A1c Is Positively Correlated with Framingham Risk Score in Older, Apparently Healthy Nondiabetic Korean Adults
- Ji Hye Shin, Ji In Kang, Yun Jung, Young Min Choi, Hyun Jung Park, Jung Hae So, Jin Hwa Kim, Sang Yong Kim, Hak Yeon Bae
- Endocrinol Metab. 2013;28(2):103-109. Published online June 18, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.2.103
- 3,817 View
- 32 Download
- 7 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Several studies have suggested that elevated levels of hemoglobin A1c (HbA1c) are associated with cardiovascular disease (CVD) in nondiabetic individuals. However, it is unclear whether HbA1c levels can serve as a simple screening marker for increased CVD risk in nondiabetic individuals. Our objective was to evaluate the relationship between HbA1c levels and CVD risk using the Framingham risk score (FRS) in older, apparently healthy nondiabetic Korean adults.
Methods We retrospectively studied 2,879 Korean adults between the ages of 40 and 79 who underwent voluntary health check-ups at the Health Promotion Center of our hospital from July 2009 to June 2011. Subjects were subdivided based on their HbA1c levels into four groups: tertiles within the HbA1c normal tolerance range and a group for subjects with an increased risk for diabetes (IRD).
Results The mean FRS for the upper tertile (9.6±3.8) group was significantly higher than that of the middle tertile (8.4±4.0) and lower tertile (7.6±3.8) groups. In addition, FRS was highest in the IRD group (10.5±3.7). Multiple linear regression analysis demonstrated that HbA1c levels exhibited a significant positive correlation with FRS when adjusted for confounding variables in all subjects (β±standard error [SE], 0.018±0.002;
R 2, 0.131), women (β±SE, 0.023±0.003;R 2, 0.170), and men (β±SE, 0.016±0.004;R 2, 0.109).Conclusion HbA1c levels were positively correlated with FRS in older, apparently healthy nondiabetic Korean adults. We propose that HbA1c levels may reflect CVD risk in nondiabetic individuals.
-
Citations
Citations to this article as recorded by- Correlation between cardiovascular risk and glycemic control among patients with diabetes
Naomi Niari Dalimunthe, Herwindo Ahmad, Dina Arwina Dalimunthe
MGM Journal of Medical Sciences.2024; 11(1): 44. CrossRef - Framingham Risk Score Assessment in Subjects with Pre-diabetes and Diabetes: A Cross-Sectional Study in Korea
Hyuk Sang Kwon, Kee Ho Song, Jae Myung Yu, Dong Sun Kim, Ho Sang Shon, Kyu Jeung Ahn, Sung Hee Choi, Seung Hyun Ko, Won Kim, Kyoung Hwa Lee, Il Seong Nam-Goong, Tae Sun Park
Journal of Obesity & Metabolic Syndrome.2021; 30(3): 261. CrossRef - Physician-Directed Diabetes Education without a Medication Change and Associated Patient Outcomes
Hun-Sung Kim, Hyunah Kim, Hae-Kyung Yang, Eun Young Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung-Hwan Lee, Jae Hyoung Cho, In Young Choi, Hyeon Woo Yim, Bong-Yun Cha
Diabetes & Metabolism Journal.2017; 41(3): 187. CrossRef - Randomized, Open-Label, Parallel Group Study to Evaluate the Effect of Internet-Based Glucose Management System on Subjects with Diabetes in China
Hun-Sung Kim, Chenglin Sun, So Jung Yang, Lin Sun, Fei Li, In Young Choi, Jae-Hyoung Cho, Guixia Wang, Kun-Ho Yoon
Telemedicine and e-Health.2016; 22(8): 666. CrossRef - GA to HbA1C ratio, but not HbA1C is associated with cognition in Chinese nondiabetic old adults
Yuan Zhong, Jun Jin, Chan Chan Xu, Guo Xiang Fu
Aging & Mental Health.2015; 19(9): 853. CrossRef - Relationship of Glycated Hemoglobin A1c, Coronary Artery Calcification and Insulin Resistance in Males Without Diabetes
Chan-Hee Jung, Eun-Jung Rhee, Kyu-Jin Kim, Bo-Yeon Kim, Se Eun Park, Yoosoo Chang, Seungho Ryu, Cheol-Young Park, Ji-Oh Mok, Ki-Won Oh, Chul-Hee Kim, Sung-Woo Park, Sung-Koo Kang, Won-Young Lee
Archives of Medical Research.2015; 46(1): 71. CrossRef - Evaluation of Nutrient Intake and Food Variety in Korean Male Adults according to Framingham Risk Score
Mi-Kyeong Choi, Yun-Jung Bae
The Korean Journal of Food And Nutrition.2014; 27(3): 484. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef - Suicidal ideation and suicide attempts among diabetes mellitus: The Korea National Health and Nutrition Examination Survey (KNHANES IV, V) from 2007 to 2012
Jae Ho Chung, Kitae Moon, Do Hyung Kim, Joo-Won Min, Tae Ho Kim, Hee-Jin Hwang
Journal of Psychosomatic Research.2014; 77(6): 457. CrossRef
- Correlation between cardiovascular risk and glycemic control among patients with diabetes

- Thyroid
- Two Cases of Methimazole-Induced Insulin Autoimmune Syndrome in Graves' Disease
- Eun Roh, Ye An Kim, Eu Jeong Ku, Jae Hyun Bae, Hye Mi Kim, Young Min Cho, Young Joo Park, Kyong Soo Park, Seong Yeon Kim, Soo Heon Kwak
- Endocrinol Metab. 2013;28(1):55-60. Published online March 25, 2013
- DOI: https://doi.org/10.3803/EnM.2013.28.1.55
- 6,381 View
- 71 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader We report here the cases of two females with Graves' disease who developed insulin autoimmune syndrome after treatment with methimazole. The patients exhibited a sudden altered mental state after treatment with methimazole for approximately 4 weeks. Patients had hypoglycemia with serum glucose below 70 mg/dL, and laboratory findings showed both high levels of serum insulin and high titers of insulin autoantibodies. The two women had never been exposed to insulin or oral antidiabetic agents, and there was no evidence of insulinoma in imaging studies. After glucose loading, serum glucose, and total insulin levels increased abnormally. One of the patient was found to have HLA-DRB1*0406, which is known to be strongly associated with methimazole-induced insulin autoimmune syndrome. After discontinuation of methimazole, hypoglycemic events disappeared within 1 month. Insulin autoantibody titer and insulin levels decreased within 5 months and there was no further development of hypoglycemic events. We present these cases with a review of the relevant literature.
-
Citations
Citations to this article as recorded by- Insulin Autoimmune Syndrome: A Systematic Review
MingXu Lin, YuHua Chen, Jie Ning, Tatsuya Kin
International Journal of Endocrinology.2023; 2023: 1. CrossRef - Safety of Antithyroid Drugs in Avoiding Hyperglycemia or Hypoglycemia in Patients With Graves’ Disease and Type 2 Diabetes Mellitus: A Literature Review
Yu-Shan Hsieh
Cureus.2023;[Epub] CrossRef - Case report: hypoglycemia secondary to methimazole-induced insulin autoimmune syndrome in young Taiwanese woman with Graves’ disease
Hsuan-Yu Wu, I-Hua Chen, Mei-Yueh Lee
Medicine.2022; 101(25): e29337. CrossRef - Analysis of the clinical characteristics of insulin autoimmune syndrome induced by methimazole
Linli Sun, Weijin Fang, Dan Yi, Wei Sun, Chunjiang Wang
Journal of Clinical Pharmacy and Therapeutics.2021; 46(2): 470. CrossRef - Preoperative plasmapheresis experience in Graves’ disease patients with anti-thyroid drug-induced hepatotoxicity
Tugce Apaydın, Onur Elbasan, Dilek Gogas Yavuz
Transfusion and Apheresis Science.2020; 59(5): 102826. CrossRef - Glycemic variation in uncontrolled Graves’ disease patients with normal glucose metabolism: Assessment by continuous glucose monitoring
Gu Gao, Feng-fei Li, Yun Hu, Reng-na Yan, Bing-li Liu, Xiao-mei Liu, Xiao-fei Su, Jian-hua Ma, Gang Hu
Endocrine.2019; 64(2): 265. CrossRef - Insulin autoimmune syndrome induced by exogenous insulin injection: a four-case series
Yimin Shen, Xiaoxiao Song, Yuezhong Ren
BMC Endocrine Disorders.2019;[Epub] CrossRef - Assessment and Management of Anti-Insulin Autoantibodies in Varying Presentations of Insulin Autoimmune Syndrome
David Church, Luís Cardoso, Richard G Kay, Claire L Williams, Bernard Freudenthal, Catriona Clarke, Julie Harris, Myuri Moorthy, Efthmia Karra, Fiona M Gribble, Frank Reimann, Keith Burling, Alistair J K Williams, Alia Munir, T Hugh Jones, Dagmar Führer,
The Journal of Clinical Endocrinology & Metabolism.2018; 103(10): 3845. CrossRef - MANAGEMENT OF ENDOCRINE DISEASE: Pathogenesis and management of hypoglycemia
Nana Esi Kittah, Adrian Vella
European Journal of Endocrinology.2017; 177(1): R37. CrossRef - Insulin autoimmune syndrome during the administration of clopidogrel
Eijiro Yamada, Shuichi Okada, Tsugumichi Saito, Aya Osaki, Atushi Ozawa, Masanobu Yamada
Journal of Diabetes.2016; 8(4): 588. CrossRef - Hyperinsulinemic hypoglycemia associated with insulin antibodies caused by exogenous insulin analog
Chih-Ting Su, Yi-Chun Lin
Endocrinology, Diabetes & Metabolism Case Reports.2016;[Epub] CrossRef - Anti-tuberculosis Treatment-Induced Insulin Autoimmune Syndrome
Jung Suk Han, Han Ju Moon, Jin Seo Kim, Hong Il Kim, Cheol Hyeon Kim, Min Joo Kim
The Ewha Medical Journal.2016; 39(4): 122. CrossRef - 2016 American Thyroid Association Guidelines for Diagnosis and Management of Hyperthyroidism and Other Causes of Thyrotoxicosis
Douglas S. Ross, Henry B. Burch, David S. Cooper, M. Carol Greenlee, Peter Laurberg, Ana Luiza Maia, Scott A. Rivkees, Mary Samuels, Julie Ann Sosa, Marius N. Stan, Martin A. Walter
Thyroid.2016; 26(10): 1343. CrossRef - Insulin Autoimmune Syndrome in a Patient with Hashimoto's Thyroiditis
In Wook Song, Eugene Han, Nan Hee Cho, Ho Chan Cho
Journal of Korean Thyroid Association.2014; 7(2): 180. CrossRef - Brief Review of Articles in 'Endocrinology and Metabolism' in 2013
Won-Young Lee
Endocrinology and Metabolism.2014; 29(3): 251. CrossRef
- Insulin Autoimmune Syndrome: A Systematic Review

- Diabetic Ketoacidosis Associated with Emphysematous Gastritis: A Case Report.
- Young Min Choi, Jun Won Seo, Woo Jin Lee, Hyeong Jin Park, Ji Hye Shin, Seung Bum Kang, Jun Lee, Jin Hwa Kim, Sang Yong Kim, Hak Yeon Bae
- Endocrinol Metab. 2011;26(4):355-359. Published online December 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.4.355
- 22,802 View
- 30 Download
-
 Abstract
Abstract
 PDF
PDF - Diabetic ketoacidosis is a serious and demanding medical emergency for the field of endocrinology, and the identification and correction of the precipitating factors is equally important. Many patients of diabetic ketoacidosis show gastrointestinal symptoms as an initial presentation, and coincidental gastrointestinal diseases can be neglected or misdiagnosed. Emphysematous gastritis is a rare and lethal disease in which gas bubbles form in the stomach wall. The predisposing factors include ingestion of corrosive substances, alcohol abuse, diabetes, and immunosuppressive therapy. Thus, it may be difficult to detect emphysematous gastritis early, especially when it is developed in conjunction with diabetic ketoacidosis. We report a case of diabetic ketoacidosis associated with emphysematous gastritis in a young male without medical history.

- Six Cases of Congenital Adrenal Hyperplasia That Were Due to 17alpha-hydroxylase/17,20-lyase Deficiency.
- Dong Hoon Shin, Sung Hoon Yu, Young Min Choi, Jung Gu Kim, Sang Wan Kim, Chan Soo Shin, Kyong Soo Park, Seong Yeon Kim
- J Korean Endocr Soc. 2009;24(2):109-115. Published online June 1, 2009
- DOI: https://doi.org/10.3803/jkes.2009.24.2.109
- 1,953 View
- 29 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - 17alpha-hydroxylase/17,20-lyase deficiency is a rare phenotype of congenital adrenal hyperplasia (CAH), and this is characterized by hyporeninemic hypertension, primary amenorrhea and abnormality of the secondary sexual characteristics (pseudohermaphroditism in men). This type of CAH is usually misdiagnosed at first as mineralocorticoid induced hypertension with primary aldosteronism, but primary amenorrhea with deficient sex hormone is a clue for making the correct diagnosis. The authors experienced 6 cases of 17alpha-hydroxylase/17,20-lyase deficiency in patients who ranged from 15 to 42 years of age. 4 cases were diagnosed according to the investigation of their mineralocorticoid-induced hypertension and 2 cases their primary amenorrhea and sexual infantilism. All of them had hypokalemia, hyporeninemic hypertension and an atrophied uterus and ovaries. In the genotypic male (46 XY), the testicles were atrophied in the abdominal cavity. The levels of cortisol, estrogen and dehydroepiandrosterone sulfate (DHEAS) were low, but the levels of progesterone and 11-deoxycorticosterone were high. Therefore, the diagnosis of 17alpha-hydroxylase/17,20-lyase deficiency should be considered in female patients who present with both sexual infantilism and mineralocorticoid hypertension. We report on these cases with a brief review of the literature.
-
Citations
Citations to this article as recorded by- Functional Identification of Compound Heterozygous Mutations in the CYP17A1 Gene Resulting in Combined 17α-Hydroxylase/17,20-Lyase Deficiency
Eun Yeong Mo, Ji-young Lee, Su Yeon Kim, Min Ji Kim, Eun Sook Kim, Seungok Lee, Je Ho Han, Sung-dae Moon
Endocrinology and Metabolism.2018; 33(3): 413. CrossRef - 17α-hydroxylase Deficiency Mimicking Hyperaldosteronism by Aldosterone-producing Adrenal Adenoma
Yun Kyung Cho, Hyeseon Oh, Sun-myoung Kang, Sujong An, Jin-Young Huh, Ji-Hyang Lee, Woo Je Lee
The Korean Journal of Medicine.2016; 91(2): 191. CrossRef
- Functional Identification of Compound Heterozygous Mutations in the CYP17A1 Gene Resulting in Combined 17α-Hydroxylase/17,20-Lyase Deficiency


 KES
KES

 First
First Prev
Prev



